Bill 2 Threatening Care for Quebec LGBTQ+, Homeless, and Vulnerable Populations
Because of Bill 2’s changes to the way doctors will be paid, at least 10 health care clinics taking care of LGBTQ+ people, the homeless, and community sexual health are likely to close in the New Year.
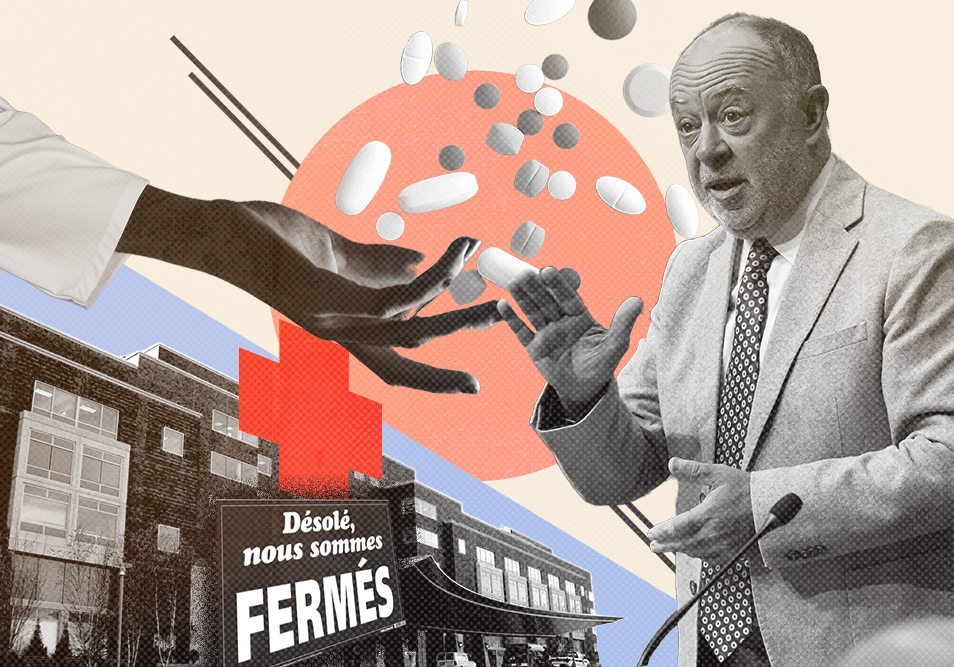
At least two renowned clinics in Montreal and eight sexual health clinics across Quebec are likely to close because of Bill 2, the provincial government’s controversial healthcare reform.
L’Agora and Quorum are located beside Berri-UQAM metro station. Both treat people with HIV, serve the LGBTQ+ community, the homeless, as well as families in the area. Prelib is a group of clinics throughout the province that help people with sexual health anonymously.
Many more Groupe de médecine de Famille (GMF) clinics beyond these are also in danger of closing, potentially causing many thousands of Quebecers to lose their family doctor.
If the bill continues as written, Dr. Maxim Régimbal-Ethier, founder of Prelib and co-founder of Quorum, says it will lead to Prelib’s immediate closure on Jan. 1, 2026. L’Agora, which often cares for people who are not registered with the provincial medicare system (RAMQ), will have to close down on April 1st unless this is quickly resolved.
The government passed the bill on Oct. 25 using a parliamentary manoeuvre that allows it to circumvent consultation with experts and opposition parties. The bill passed against the advice of doctors across the province, which quickly led to one of the party’s cabinet ministers stepping down, 260 doctors looking to leave the province, and an onslaught of bad press for the already struggling government in what is likely its final year.
“The law is generating a lot of reactions, and that’s normal,” a spokesperson for the Ministère de la Santé et des Services sociaux (MSSS) said. “The goal of the law is to increase access.”
Under the new rules in Bill 2, the government is threatening to remove a large portion of payments, up to 15 per cent, to doctors based on yet-to-be-defined parameters.
Dr. Emmanuelle Huchet, the director of l’Agora, explained that future payments will also be based on patient categories: green, yellow, and red. These colours indicate whether a patient is low, medium, or high priority. The payments could vary significantly depending on whether a patient is severely ill, or if they are less ill.
The government has not indicated which colours correspond to sexual health or homelessness, despite several emails from the doctors requesting clarification. If sexual health is ranked lower on this payment scale, it will severely affect the income of all these clinics.
The payment seems to prioritize the number of people seen over the quality of service they receive by discouraging practitioners from spending time with patients. The government has outlined the need for doctors to spend no more than 15 minutes with each patient to improve efficiency.
“We can’t keep these clinics afloat on a shoestring, and clearly, it’s not working,” said Régimbal-Ethier.
Support your local indie journalists.
“Under Bill 2, I have to report on my colleagues. (I have to say) ‘How many patients did you see today? Why was there an empty space in the schedule? Why didn’t you see a patient from one o’clock to two o’clock?’” Huchet said. If she doesn’t send this report in, she incurs a $2,000 fine every single week.
The new regulations will cut payments for Prelib. They contacted the government, which said “they understand the uncertainty” and several elements from Bill 2 “remain to be agreed upon.”
Prelib provides rapid, anonymous sexual health assistance and has become an essential resource for people who are unable or unwilling to go to traditional clinics. These clinics help almost 100,000 per year. According to data from Santé Québec, there were about 35,000 screening tests done. Some 22,963 STI screening tests among people aged 14 to 25 were carried out last year in public SIDEP clinics. In the same age group, Prelib performed 19,883 tests. Several other private clinics also offer STI screening, so this seems to indicate that the total number of tests in this age group exceeds 35,000 per year.
“We help sex workers, transgender people, and drug users. We’re taking a broad approach to promote access to sexual health, to create truly inclusive environments,” Régimbal-Ethier said.
His other clinic, Quorum, is also in danger of shutting down. Bill 2 cares about efficiency, but Quorum has a clientele that is predominantly transgender, gay, and often sex workers, who need more time and have a level of trust that they don’t feel in many other places. Régimbal-Ethier said that the clinic handles more sensitive situations and that the bill will cut into its mandate.
“On Jan. 1, 15 per cent of our remuneration will be based on ‘performance indicators.’ But what are these?” said Huchet, the director of l’Agora. The government replied to her that it hadn’t made that decision, but whatever they are, they will be in place on Jan. 1. Huchet is exasperated.
“Well, Jan. 1 is six weeks away!”
The government rejected that the stipulations in the bill are ‘performance indicators’ and told The Rover they were “national, territorial or local objectives” that have to be achieved.
“We understand the concerns raised,” a spokesperson for the health ministry said. “That’s why we organized a webinar last week to clarify the law.”
“We got nothing from the webinar. It made me sick to my stomach!” Huchet said. She said they didn’t take questions during the webinar, only by writing, and few clarifications have been made since.
Her clinic, l’Agora, tends to many unregistered people without a RAMQ card. RAMQ pays per patient seen. Despite often not receiving income, the clinic has taken it on its shoulders to serve the homeless and many refugees who do not have access to RAMQ. L’Agora has hired extra staff on its own dime, such as a social worker and extra nurses, because of the challenging nature of its clientele.
The government declared the clinic a “pilot project” and has provided some funding to care for this unregistered clientele, but has not confirmed the continuation of this program. So far, funding has been spotty and inconsistent. It has taken up to six months for the funds to arrive, which the clinic is not able to consistently endure.
Furthermore, doctors have to report their staff to the government for not being ‘busy enough.’
“Under Bill 2, I have to report on my colleagues. (I have to say) ‘How many patients did you see today? Why was there an empty space in the schedule? Why didn’t you see a patient from one o’clock to two o’clock?’” Huchet said. If she doesn’t send this report in, she incurs a $2,000 fine every single week.
“I worked in the system when it was healthy. But over time, everything became heavy, complex,” Huchet said. She believes the system became more about bureaucracy than quality service. Full workdays have to be devoted to administrative tasks every single week, when they already have automated systems that the government doesn’t accept. The staff at l’Agora feel that the government prioritizes statistics over results.
“We have the means to automate these stats easily,” Xavier, a nurse at l’Agora, said. With their current systems, everything is automated, but then they have to fill everything out by hand as well.
“This is precisely why we launched a series of measures to reduce the administrative burden on doctors,” a spokesperson for the ministry said. “Recent announcements will free up nearly 590,000 medical appointments per year by eliminating tasks with no clinical value.” The ministry points to Bill 68, which removed the requirement for doctors to provide medical notes for short absences and receive insurance for their prescriptions.
Xavier, a nurse at the clinic, said there have been occasions when someone’s life was clearly in danger, yet they chose to go to l’Agora instead of the emergency room because of the trust they shared.
“I thought to myself… this guy looks like he might die! Why is he here?” Xavier said. “It’s the trust we have from the patients… at some point you get used to it. We see a lot of patients, and we know them, and we try to help them.”
Huchet doesn’t know the way forward for the clinic. A patient told Huchet that l’Agora is the only place where he doesn’t feel judged or questioned.
“When he came for his appointment, he told me, ‘I’m going to come and unburden myself here.'” Huchet said.
As of April 1, that might no longer be possible.



“The government has outlined the need for doctors to spend no more than 15 minutes with each patient to improve efficiency.” As someone who’s job has been changed from “help people understand” to “you should focus on only have 11-minutes-or-less calls and tell them to call back if they need more help” i can confirm that this has had the opposing effect.
1- People are more angry at us because they feel like we just want to get rid of them after waiting for hours to reach us,
2- the wait times are still just as high,
3- the stress level of the employees has only gone up,
4- the actual service delivered has gone drastically down quality
Which frankly are all things i do not want to see in the healthcare system. I currently can’t get an appointment for a follow up bloodwork because my doctor retired and the ones at the GAP don’t do follow up, this is going to make millions of people more susceptible to develop illnesses that could have been preventable with a family doctor, but this government decided that only the rich gets to be treated, and it’s despicable.
Also can we talk about this whole culture of needing your employees to be busy all the time and increased surveillance in the workplace? It’s not healthy. We’re being slowly acclimated to it, like frogs in warming water, first it was for people working service jobs, like couche-tard and McDonald’s, then it went into office workers, now it’s spreading to medicine! Humans aren’t machines! We cannot be as good all the time if we don’t have a small respite here and there, and i feel like I’m not hearing enough conversation about this in my day to day. Even my coworkers found it normal when we were told our screens would be recorded to help increase efficiency. This needs to stop.